Formative Years
Polio: Part I
by John S. Emrich and Charles Richter
December 2020
In the late 19th century, sporadic outbreaks of a perplexing and debilitating disease began to appear in both the United States and Europe. Most of those affected, primarily young children, would experience a fever and perhaps some pain or stiffness and then recover. But in a small percentage, the disease would progress to paralysis of legs or the diaphragm, sometimes leading to death. Poliomyelitis, or simply polio, presented medical researchers and early immunologists with special problems that grew more urgent as outbreaks became epidemics and the effects of the disease more severe. From its inception, The Journal of Immunology (The JI) published some of the most important research on the nature of polio, ultimately leading to the successful vaccines of the 1950s.
The Discovery of Viruses
Although polio seemed like a new plague at the dawn of the 20th century, evidence of its paralytic effects can be traced to ancient Egypt and ancient Greece. This disease was rare and, to all appearances, random and therefore not well understood until shortly after the discovery of viruses in the late 19th century.
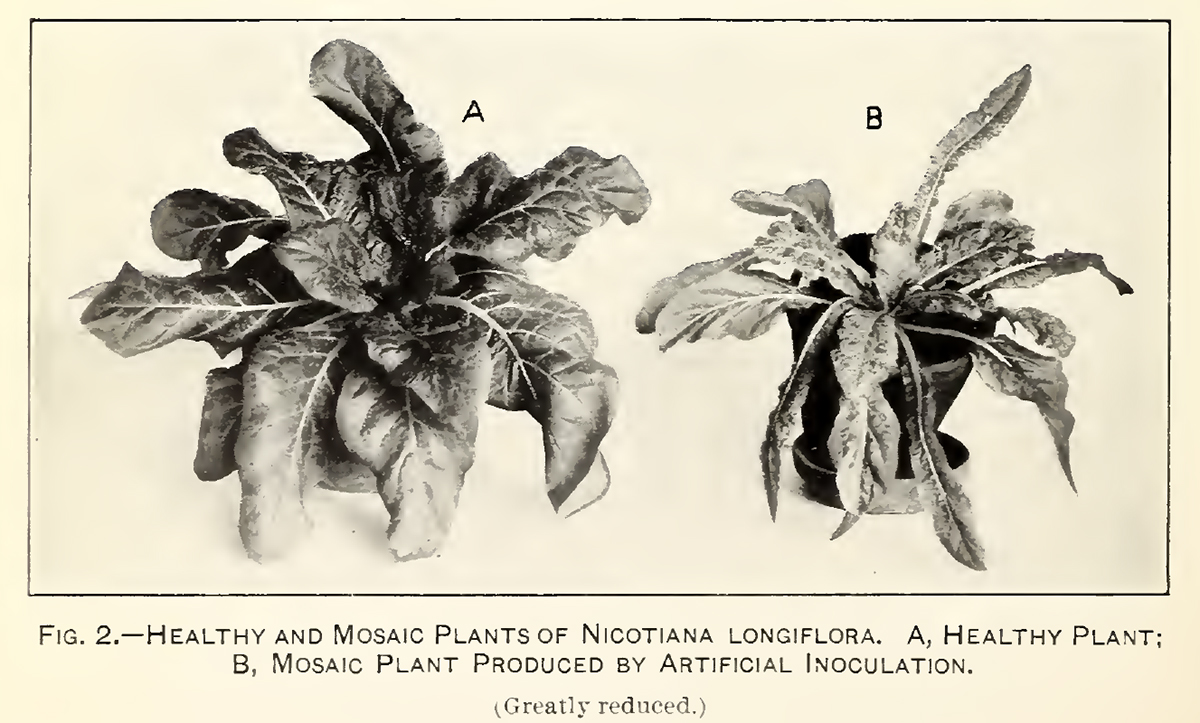 TMV symptoms, 1914
TMV symptoms, 1914
USDABacteria were first seen by the naked eye with the invention of the microscope by Antonie Van Leeuwenhook in 1668; soon thereafter the field of bacteriology was born. Virology came much later because the causative agents could not be seen even under the highest powered light microscope.
The term virus (“poison” in Latin) had been used for centuries to describe medical maladies for which the cause was mysterious. The imprecision of the term, however, would end with the 1898 discovery of he tobacco mosaic virus (TMV), an infectious agent that could be spread through the sap of the tobacco plant. The experiment underlying the discovery was rather straightforward and owed its success to the porcelain Chamberland filter, which had pores so small that a solution that passed through it would be bacteria free.
Typically, the filter was used to strain out bacteria to be tested. However, when a pasteurized aqueous solution containing crushed-up leaves of diseased tobacco plants was forced through the filter, the remaining solution could still infect tobacco plants. Though the TMV was not seen, nor could it be grown in laboratory cultures, it was the first “filterable virus” to be isolated.
Many more viruses were soon isolated. The first vertebrate virus, foot-and-mouth, was isolated in 1898, and the first human virus, yellow fever, was isolated in 1900. And in 1935, Wendell M. Stanley (AAI 1957) was the first to crystalize a virus—the TMV—and demonstrated that it was composed of protein and ribonucleic acid. He was awarded the Nobel Prize in Chemistry in 1946 for his research.
Polio Outbreaks
In the mid-1800s, doctors were reporting clusters of infantile paralysis during the summer months in the United States and Western Europe, though the clusters were so small and sporadic that uncovering a clinical diagnosis for the disease was impossible. The first epidemic in the United States occurred in the Otter Valley of Vermont during the summer of 1894.
 Charles Caverly
Charles Caverly
Rutland HeraldCharles Caverly, a diligent local doctor, was able to trace the 123 people comprising the Vermont cases and noted the sex, age, symptoms, and outcome for each. Though unable to determine the cause of the disease, he laid the groundwork by reaching three important conclusions: polio had the potential to become an epidemic; most of the victims were children, not infants, thus “infantile paralysis” was a misnomer; and some victims experienced an extremely mild form of illness with minor symptoms and a quick recovery.
In July 1904, the world’s first major epidemic of polio began in Sweden. The countryside around Stockholm had seen outbreaks of polio sporadically over the previous three decades, with the most recent in 1895. The 1904 epidemic began in a small village 155 miles southwest of Stockholm. Within three months, cases had been reported in nearly every county in the country. In August alone, 360 cases were reported, and by year’s end there was a total of 1,031.
A majority of the cases became the subject of a comprehensive survey by Ivar Wickman, who crisscrossed the country to get detailed accounts from victims and families. His conclusions reinforced Caverly’s hypotheses, vastly expanding the understanding of the disease: it was spread through personal contact; all infected persons, symptomatic and asymptomatic, were contagious; and the incubation period for first symptoms was three to four days after infection and a further six to eight days for paralysis.
The number of polio epidemics increased in number and severity into the 20th century, and with each epidemic, understanding of the disease increased incrementally. The causative agent, however, remained a mystery.
The Polio Virus
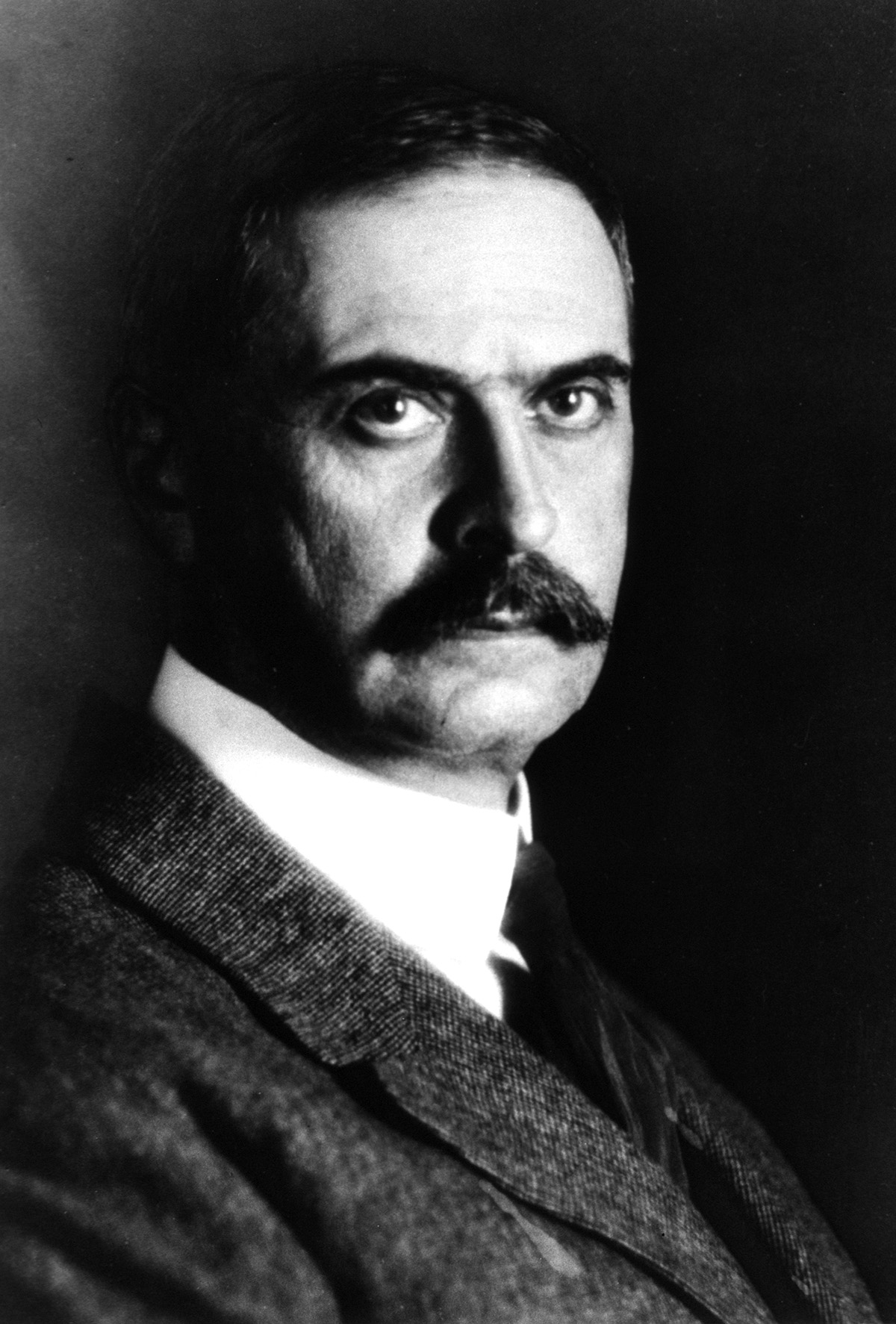 Karl Landsteiner
Karl Landsteiner
National Library of MedicineOn December 18, 1908, Karl Landsteiner (AAI 1922, president 1927–28) rose to give a talk at the Royal and Imperial Society of Physicians in Vienna. The topic of his talk was polio, and he was there to announce that he had isolated the filterable virus responsible for the disease. Landsteiner had taken a sample from the inflamed spinal cord of a child recently claimed by the disease, ground it up in sterile water, and injected it into guinea pigs, rabbits, and mice to no avail. Then he injected samples into the abdomen of two monkeys. The first died after eight days, and the second became paralyzed from the waist down before dying on Day 18 post-infection. The spinal cords of both monkeys exhibited the telltale lesions of polio. Further research using filtrates yielded identical results. The polio virus had been isolated.
Flexner and Early Polio Research in the United States
Back in the United States, Simon Flexner (AAI 1920), the director of the recently opened Rockefeller Institute for Medical Research (RIMR) and editor-in-chief of the Journal of Experimental Medicine, had begun his own polio research. By 1907, the country was also experiencing an increase in outbreaks both in number and severity during the summer months. That year, New York City health officials reported 2,000 cases, and similar outbreaks were reported in Massachusetts, Minnesota, Nebraska, Ohio, Wisconsin, and Vermont.
 Simon Flexner
Simon Flexner
National Library of MedicineLater, after successfully reproducing Landsteiner’s work, Flexner began a series of experiments to determine where the virus entered the body. And like Landsteiner and many other researchers, Flexner was using a monkey model for the disease.
This choice in model had its positives and negatives. Monkeys were able to be infected by polio, though not naturally. Like today, they were expensive and difficult to buy and maintain; by contrast, at the time of Flexner’s research, the origins and previous conditions of the monkeys were usually completely unknown.
Flexner’s research into the entry point for the virus began with feeding his test subjects poliovirus by mouth. None got sick. Next, he introduced the virus into their sinuses by using a swab dipped in filtrates and watched as the monkeys soon became sick. Flexner reasoned, incorrectly as it turned out, that the virus entered through the nose and traveled into the central nervous system.
By 1911, an optimistic Flexner was quoted in the New York Times saying, “We have already discovered how to prevent infantile paralysis” and that the “achievement of a cure, I may conservatively say, is not now far distant.”
What later research would show was that, unbeknownst to Flexner, his selection of a Macaca mulatta (rhesus monkey) was the fatal flaw in his research because that species is unable to orally contract polio.
The 1916 Polio Epidemic
The year 1915 proved relatively unremarkable for New York City public health officials; in terms of public health, the numbers were very similar to those in 1914. While deaths brought on by the prevailing endemic communicable diseases remained relatively constant in 1915, the maladies remained a daily threat to the nearly five million residents of the city. The top pathogen-related deaths included pneumonia (10,692), tuberculosis (10,321), diphtheria (1,271), measles (662), influenza (394), whooping cough (395), typhoid fever (327), and scarlet fever (310). There were no vaccines or effective therapeutics for any of these, and readily available laboratory testing existed for only a few.
 Brooklyn, NY, 1914
Brooklyn, NY, 1914
New York Historical SocietyThe biggest event in the city that year was the women’s suffrage parade down Fifth Avenue on October 23. The official counts for the gathering ranged from 25,000 to 60,000 participants and at least 100,000 spectators. Polio would have caused little worry to residents of the city’s five boroughs, young or old, as only 70 deaths had been attributed to the disease in the entire state.
Across the United States in 1915, only 691 reported deaths were caused by polio, of which the vast majority were children under the age of five. As winter waned into the spring of 1916, there was no warning that New York City was soon to become ground zero for the first major outbreak of polio in America.
The first issue of The JI came out just three months before cases of polio started appearing in May of 1916 in a densely populated section of Brooklyn known as Pigtown. By year’s end, the disease would claim the lives of more than 6,000 people, mostly children, and leave another 21,000 with permanent physical disability. This first major American epidemic of polio hit the New York City area hardest: about 9,000 children were affected, and 2,343 of them died.
At the time, very little was known about how polio was transmitted or how to prevent infection. Because only about one percent of infected patients experience paralytic symptoms, the virus seemed less contagious than it actually was, and public health officials had difficulty identifying routes of transmission. Medical and government authorities instituted sanitation drives, food inspections, and even travel bans for children. Treatment options were limited during the epidemic as well. By the time polio had caused paralysis in a child, all a physician could do was prescribe medication to treat the pain and fever. The iron lung had not yet been developed to treat cases of respiratory paralysis.
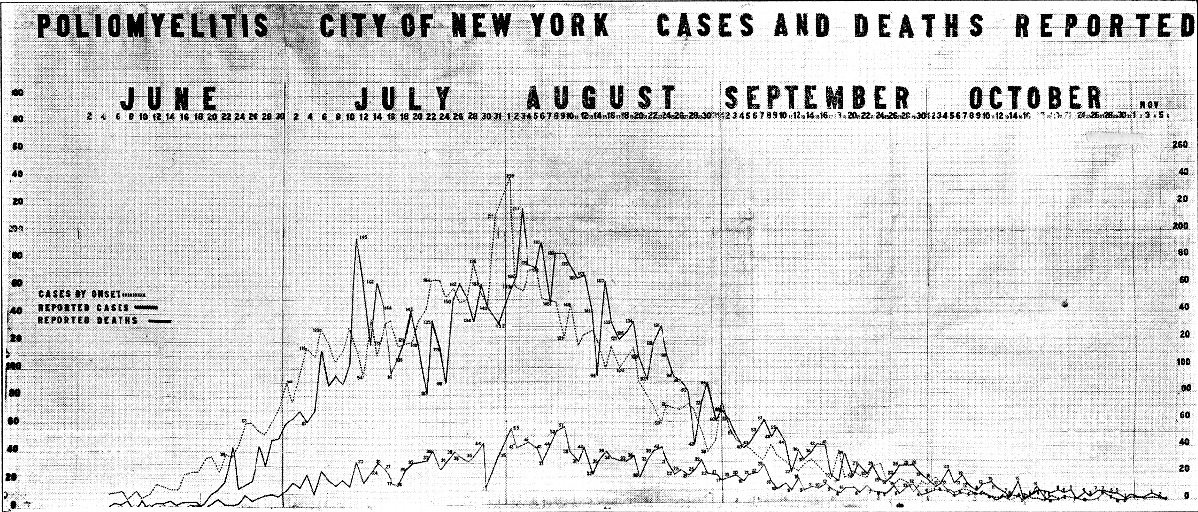 NY polio epidemic, 1916
NY polio epidemic, 1916
NY Dept. of Health
A Catalyst for AAI Researchers
Many of the earliest AAI members would have witnessed the New York polio epidemic firsthand. Thirteen members, including Arthur F. Coca (AAI 1916, EIC 1916–1935), William H. Park (AAI 1916, president 1918–19), James W. Jobling (AAI 1914, president 1915–16), and Richard Weil (AAI 1914, president 1916–17), lived in New York City during the summer of the outbreak. Another six New Yorkers would join AAI in the ensuing year, including Hans Zinsser (AAI 1917, president 1919–20) and Peter K. Olitsky (AAI 1917).
 Polio health pass, 1916
Polio health pass, 1916
Smithsonian, NMAHThe 1916 epidemic inspired new research on polio, and in its early years, The JI published important articles that built on the previous discoveries of Landsteiner and Flexner. At this point, it was still very challenging to work with polio because the virus could not be successfully cultured in vitro. Monkeys were the only experimental animal that the virus would reliably infect, making experiments expensive as well.
John Kolmer (AAI 1913, president 1917–18) published the first article on polio in The JI with Anna E. Freese. Hoping that a complement-fixation diagnostic could be developed for polio as had been done for syphilis, they used samples of cerebrospinal fluids and blood sera from patients in different stages of polio infection to determine (1) whether specific antigen could be detected in corresponding tissues, and (2) whether antibodies for “various and easily cultivated” bacteria could be demonstrated. Unfortunately, their research showed that the Wassermann reaction was uniformly negative for acute anterior poliomyelitis. They found that though there was some evidence of complement fixation with polio serum, the reactions were too insignificant to be used as a practical diagnostic.
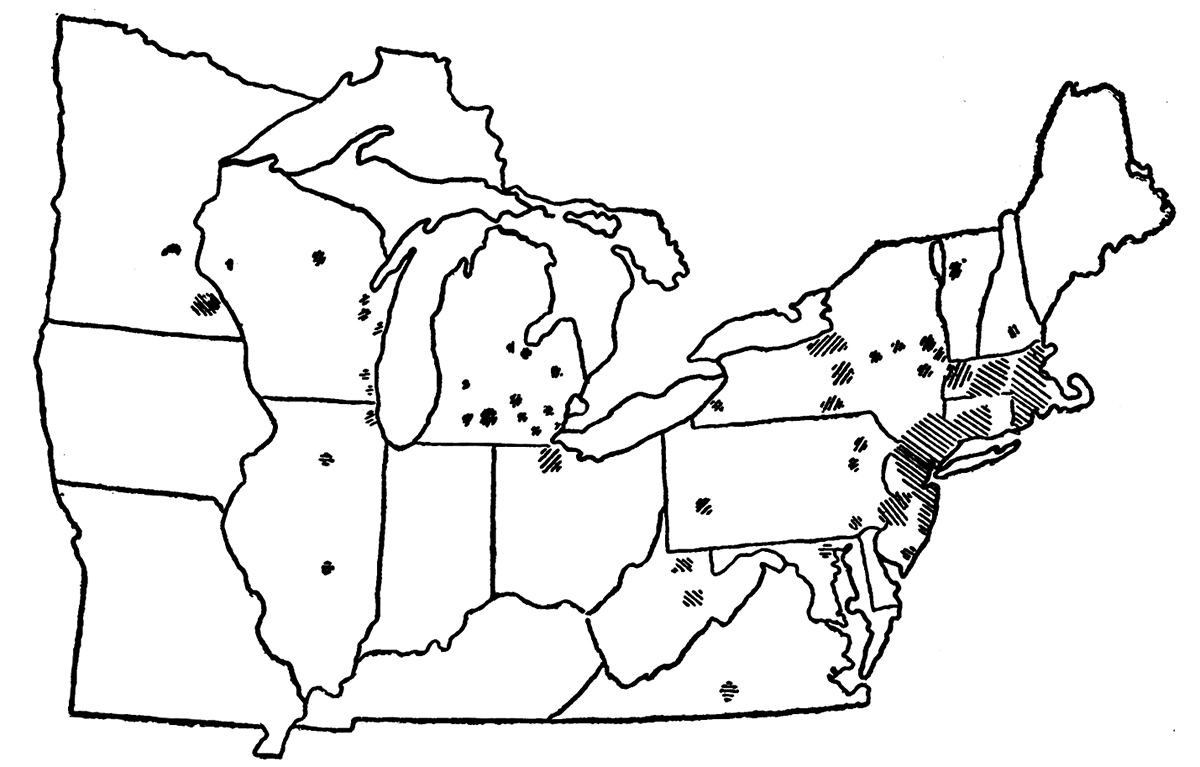 Polio epidemic map, 1916
Polio epidemic map, 1916
Public Health ReportsSeeing similarities between the polio and rabies viruses, H. L. Abramson (AAI 1918) and Herman Gerber of the New York Department of Health tried to produce a vaccine based on those analogous properties. They conducted experiments to determine if a highly potent strain of polio isolated at RIMR could be attenuated either chemically or with heat, as with rabies.
Attenuation with formalin proved “decidingly not encouraging,” so they turned to heating methods. Abramson and Gerber showed in monkeys that a course of five injections of the heat-treated virus over five days could produce substantial immunity to the potent virus when introduced later.
A Return to Polio Research
Polio continued to plague American children: 1921 and 1925 had significant spikes in cases and deaths, and 1927 was the worst year since 1916. After a gap of almost 10 years, polio research in The JI picked up again with wide-ranging approaches to understanding immunity to the disease. In 1927, W. Lloyd Aycock and J. R. Kagan reviewed the state of polio vaccine science and showed that it was possible to produce immunity without active symptoms.
The Kolmer and Brodie Vaccine Trials
By 1934, research had advanced sufficiently to make the first serious human trials possible. As in the case of the competing Salk and Sabin vaccine efforts that would come later, two scientists independently developed initial polio vaccines, one using killed virus and one using attenuated. John Kolmer attenuated the virus with sodium ricinoleate to produce a vaccine. Monkey tests looked promising, so he then tested his vaccine on himself and his assistant with no ill effects. Kolmer quickly moved to tests on children. His own sons received it first, and then he distributed it to physicians across the country. In September 1935, he reported that 10,725 children had been given the vaccine, and none who had received all three doses had contracted polio. There were, however, nine cases in children who had only one or two doses.
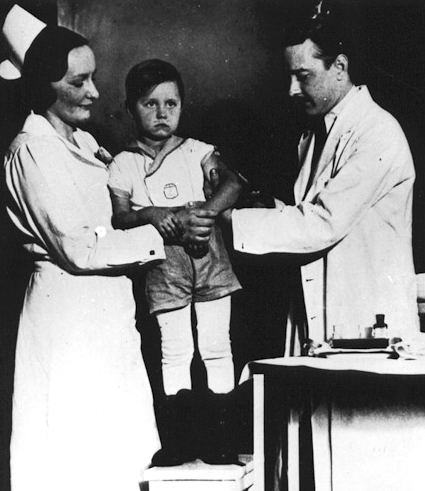 Kolmer injecting son with polio vaccine, 1935
Kolmer injecting son with polio vaccine, 1935
Detroit NewsAlso in 1934, Maurice Brodie (AAI 1934) began work on a polio virus in the Bureau of Laboratories of the New York Department of Health under William H. Park. Using formalin-killed virus, he produced humoral immunity in monkeys reliably, but tissue immunity in only a few (a live virus had the opposite ratio). The common belief at the time was that tissue immunity was the more important component of protection from the virus. Like Kolmer, Brodie swiftly moved to human trials on more than 4,500 children. He also reported five cases of polio among the vaccinated subjects, but two of those children had been exposed just prior to receiving the vaccine, and another only 13 days after getting just a single dose.
Now there were two vaccines that offered the promise of bringing an end to the scourge of polio. Sidney Kramer made a large comparative study to verify efficacy of these two vaccines, funded partly by the President's Birthday Ball Commission for Infantile Paralysis Research, the original precursor to the March of Dimes. The study showed that neither vaccine was significantly more effective than a control. Kramer cited private correspondence in which Kolmer said that he no longer believed that sodium ricinoleate actually attenuated the virus.
At the 1935 American Public Health Association annual conference, both vaccines were denounced as ineffective or dangerous. Brodie acknowledged the failure of his work in person. Ultimately, however, Brodie’s vaccine did produce immunity in children comparable to the natural immunity of adults (75 percent), but the concerns raised in 1935 by the scientific community effectively barred further research at the time. Much later research suggests that the cases of polio in children who received Kolmer’s vaccine may have been provoked by the monkey spinal cord antigens, which were present due to the production method of the vaccine and not from the introduced virus itself.
In the ensuing years, polio remained a significant problem in the United States, with most years seeing 4,000 to 10,000 cases. The numbers began skyrocketing in 1943, but by that time the outbreak of the Second World War had funneled research away from diseases such as polio in favor of studies addressing the immediate needs of the war.
See also articles that were part of this series:
References
- Abramson, H. L. and Herman Gerber. “Active Immunity in Experimental Poliomyelitis.” The Journal of Immunology 3, no. 6
- Alcock, W. Lloyd and J. R. Kagan. “Experimental Immunization in Poliomyelitis.” The Journal of Immunology 14, no. 2.
- Berk, Lawrence B. “Polio Vaccine Trials of 1935.” Transactions & Studies of the College of Physicians of Philadelphia Ser. 5, vol. 11, no. 4.
- Flexner, Simon and Paul A. Lewis. “The Transmission of Acute Poliomyelitis to Monkeys.” Journal of the American Medical Association 53 no. 20: 1639.
- Flexner, Simon and Paul A. Lewis. “The Transmission of Acute Poliomyelitis to Monkeys: A Further Note.” Journal of the American Medical Association 53 no. 23.
- Hitchcock, Laurel Iverson and Paul H. Stuart. “Pioneering Health Care for Children with Disabilities: Untold Legacy of the 1916 Polio Epidemic in the United States.” Journal of Community Practice 25, no. 1.
- Kolmer, John A. and Anna E. Freese. “Complement Fixation in Acute Anterior Poliomyelitis.” The Journal of Immunology 2, no. 3.
- Kolmer, John A. and Anna M. Rule. “Concerning Vaccination of Monkeys Against Acute Anterior Poliomyelitis, with Special Reference to Oral Immunization.” em>The Journal of Immunology 26, no. 6.
- Kolmer, John A. and Anna M. Rule. ““Active Immunization Against Acute Anterior Poliomyelitis with Ricinoleated Vaccine.” The Journal of Immunology 32, no. 5.
- Kramer, S. D. “Active Immunization against Poliomyelitis. A Comparative Study I. Attempts at Immunization of Monkeys and Children with Formalized Virus.” The Journal of Immunology 31, no. 3.
- Kramer, S. D. “Active Immunization against Poliomyelitis. A Comparative Study II. Experimental Immunization of Monkeys with Virus Treated with Sodium Ricinoleate.” The Journal of Immunology 31, no. 3
- Oldstone, Michael B.A. Viruses, Plagues, and History: Past, Present, and Future. New York: Oxford University Press, 2010.
- Oshinsky, David M. Polio: An American Story. New York: Oxford University Press, 2005.
- Rogers, Naomi. Dirt and Disease: Polio Before FDR. New Brunswick: Rutgers, 1992.
- Rogers, Naomi. “Dirt, Flies, and Immigrants: Explaining the Epidemiology of Poliomyelitis, 1900–1916.” Journal of the History of Medicine and Allied Sciences 44, no. 4.
- Trevelyan, Barry, Matthew Smallman-Raynor, and Andrew D. Cliff. “The Spatial Dynamics of Poliomyelitis in the United States: From Epidemic Emergence to Vaccine-Induced Retreat, 1910–1971.” Annals of the Association of American Geographers 95, no. 2.
- U.S. Department of Commerce, Bureau of the Census. Mortality Statistics, 1915, Sixteenth Annual Report. Washington, DC: Government Printing Office, 1917.
- Williams, Gareth. Paralyzed with Fear: The Story of Polio. New York: Palgrave Macmillian, 2015.
- Williams, Greer. Virus Hunters. New York: Alfred A. Knopf, 1959.
- Wyatt, H. V. “Poliovaccines: Lessons Learnt and Forgotten.” History and Philosophy of the Life Sciences 17, no. 1.
- “Near to a Cure for Infantile Paralysis.” New York Times. 9 March 1911.