The Geography of Immunology
The Emergence of Immunology in Pittsburgh
by Bryan Peery and John S. Emrich
March/April 2015, pages 14–19
With IMMUNOLOGY 2014™ taking place in Pittsburgh, Pennsylvania, May 2–6, AAI salutes the current prominence of this city in biomedical research and reflects on the individuals and events contributing to its emergence as an international center for immunology.
Pittsburgh, a major center for immunological research, began its steep ascent to that acclaim just 60 years ago when it attracted a few ambitious, young immunologists to the University of Pittsburgh (Pitt). Among the scientists who arrived in the late 1940s and 1950s were several distinguished members of the American Association of Immunologists (AAI), including Jonas Salk (AAI '47), Frank Dixon (AAI '50, president 1971–72), F. Sargent Cheever (AAI '50, president 1963–64), and Niels Jerne (AAI '65). We chronicle below the achievements of these and other leading immunologists and their roles in shaping the history of immunology in Pittsburgh.
Early Medical Research in Pittsburgh
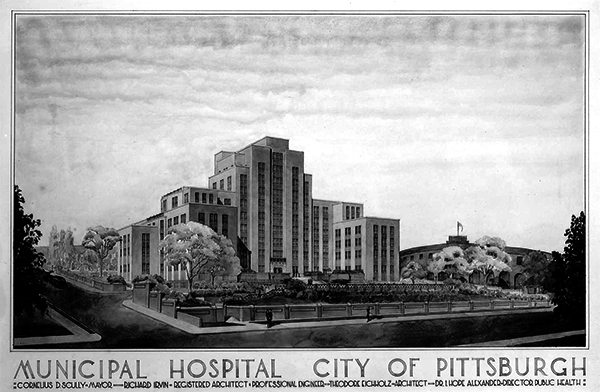 Pittsburgh Municipal Hospital, 1939
Pittsburgh Municipal Hospital, 1939
University of PittsburghThe discovery of large coal veins in 1833 brought rapid industrialization to Pittsburgh. The transformation of Pittsburgh from a small frontier city to an industrial center was accelerated by the mass production of steel and the heightened demand for that product during the American Civil War.
The city’s prominence in higher education and medicine, however, experienced a slower emergence. Western University of Pittsburgh was incorporated in 1813 but lacked a sizable enrollment until the turn of the twentieth century. It was not until 1853, following a decade that witnessed endemic typhoid and tuberculosis, as well as multiple outbreaks of smallpox and cholera, that the first chartered public hospital, Western Pennsylvania Hospital, opened its doors. A group of local physicians chartered the first medical school in 1883, and construction began after 250 shares of stock were sold for $100 each. Western Pennsylvania Medical College opened its doors to the first class in 1886. Initially, the college was completely autonomous, but in 1892, it entered into a formal relationship with Western University, officially becoming the Medical Department of Western University, although it was the stockholders, not the university, who had ownership and authority over the department.
Western University underwent dramatic changes in 1908 to raise both the standards and prominence of the school. A new name—the University of Pittsburgh—was adopted, the campus was relocated from its site in Pittsburgh’s North Side section to the Oakland area of the city, and the university formally acquired the medical college. With full control of what was now the University of Pittsburgh School of Medicine, the administration of Pitt hired a new chancellor, Samuel McCormick, who, modeling the institution on the top medical schools in the country, began recruiting accomplished researchers for faculty positions and raising the standards for enrollment and graduation. Facilities and opportunities for clinical research followed, as a new medical school building was opened in 1911, and formal relationships were forged with St. Francis and Mercy hospitals in 1912.
The University of Pittsburgh School of Medicine was not the only medical research institution in the city in these years. The William H. Singer Memorial Research Laboratory was founded at Allegheny General Hospital in 1914 as a research laboratory dedicated to the study of medical and surgical problems. Its staff included Oscar M. Teague (AAI '20), a noted bacteriologist and the first active AAI member in Pittsburgh, as well as other researchers, who, although not AAI members, published early articles in The Journal of Immunology (The JI). Western Pennsylvania Hospital also attracted talented immunologists beginning in the 1910s: Jacques J. Bronfenbrenner (AAI '20, president 1942–46) was director of research and diagnostic laboratories at Western Penn from 1913 to 1917, and Arthur P. Locke (AAI '26) and Ralph R. Mellon (AAI '22) were researchers in the laboratories from the 1930s until the 1950s.
The stature of the medical research in Pittsburgh steadily increased from the 1910s through the mid-1940s, but a series of events—the First World War, the Great Depression, and the Second World War—delayed more rapid progress until the end of the 1940s.
Post-War Pittsburgh Renaissance
Turning the University of Pittsburgh School of Medicine into a first-rate research institution had been William S. McEllroy’s aspiration since his election as dean by the medical school faculty in 1938. Born into an affluent Pittsburgh family, McEllroy had personal connections to Pittsburgh’s private donors who might turn his dream into a reality.
Resources and focus for McEllroy’s plan were soon diverted to the U.S. war effort following the December 7, 1941, attack on Pearl Harbor. With the war’s end in 1945, however, McEllroy and Pitt benefitted from the financing and enthusiasm of industrialists and philanthropists united in efforts to usher in “the Pittsburgh Renaissance.” Their plan for revitalizing the city included drastically improving public health. McEllroy encouraged the university chancellor to use a portion of the new endowment to fund a university-wide interdisciplinary research program known as the Division of Research in the Natural Sciences. Furthermore, in 1948, the Graduate School of Public Health was founded at Pitt with a $13.6 million endowment from the Andrew W. Mellon Education and Charitable Trust. McEllroy sought to make sure the medical and public health schools’ interests were closely aligned. He found an ally in the dean of the new public health program, former U.S. Surgeon General Thomas Parran, Jr., who argued that the success of the Graduate School of Public Health would depend on the School of Medicine’s receiving the investment necessary to become a top-light institution.
With financial backing and the new Division of Research serving as an indicator of the direction in which Pitt was heading, McEllroy began recruiting researchers from around the country. Convincing established scientists to tie their fates to the nascent program proved difficult because the appointments lacked status. Younger scientists, however, could be attracted by the promise of independence and a unique opportunity to expedite their advancement through the academic ranks. One researcher who was looking for just such an opportunity was Jonas Salk.
Jonas Salk and Polio Research at Pitt
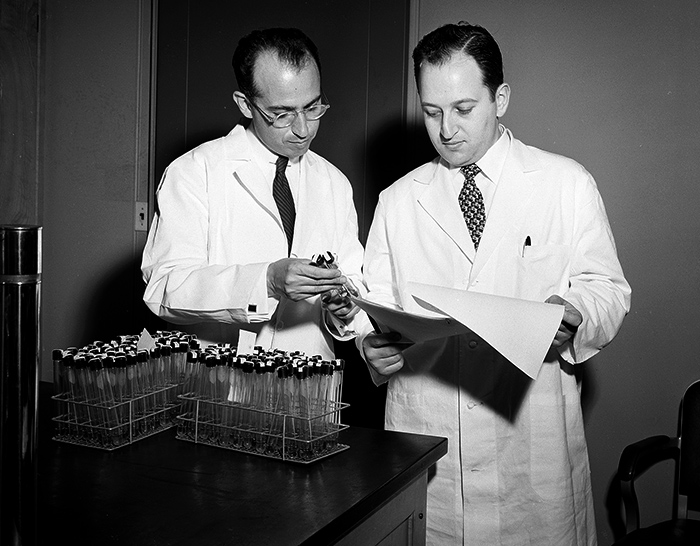 Jonas Salk and Julius Youngner, c. 1954
Jonas Salk and Julius Youngner, c. 1954
University of Pittsburgh News ServicesAfter the war, McEllroy, recognizing virology as a young but promising field that might soon put Pitt on the map, began fundraising for virus research. In 1946, he secured funds from the National Foundation for Infantile Paralysis (NFIP) to start a Virus Research Laboratory. His search for a director of the new laboratory led him to an assistant professor of epidemiology at the University of Michigan School of Public Health, Jonas E. Salk.
Although Salks’s credentials were respectable, he was hardly a luminary in 1947, and there was little to indicate that he would become the legend that he is today. The eldest son of working-class Russian immigrants, Salk grew up in the Bronx, New York, and attended City College of New York during the Great Depression before earning his M.D. from the New York University (NYU) College of Medicine in 1939. At NYU, he studied under William H. Park (AAI '16, president 1918–19) and Thomas Francis, Jr. (AAI '30, president 1949–50), who was then experimenting with using ultraviolet light to produce killed-virus vaccines. After completing a two-year medical internship at Mount Sinai Hospital in New York, Salk contacted Francis in 1942 about a job. The previous year, Francis had become chair of the Department of Epidemiology at the University of Michigan School of Public Health and director of the Influenza Commission of the Armed Forces Epidemiological Board. Francis brought Salk to Michigan, helping Salk secure both a National Research Council Fellowship and a draft deferment.
After five years under Francis, Salk grew restless, desiring a promotion and more independence. He and Francis had a cordial relationship, but Francis could offer only an assistant professorship. When McEllroy promised to make Salk an associate professor and head of the Virus Research Laboratory at Pitt in 1947, he immediately accepted the offer.
At the time of Salk’s arrival in Pittsburgh, the medical school’s transition to major research institution was far from complete. Salk soon realized that it fell upon him to be an impetus for change. He later recalled the shock of learning that most of his colleagues “were part- time instructors who earned their living in private practice and had neither the time nor inclination for basic research.” He would have to build his laboratory from the ground up—literally. Starting with two rooms and a technician in the basement of Municipal Hospital, he waged what one colleague recalled as “a kind of guerilla war” for space and funding.
He continued his investigations into influenza virus but increasingly turned to poliomyelitis virus, at least in part because he knew this research would attract funding. When NFIP approached him in late 1947 about doing the tedious technical work of typing poliovirus, Salk readily agreed to do what senior researchers had shunned. In return, he received large research grants, beginning in 1948, to help him build his laboratory. By 1949, his laboratory and offices had expanded to two floors in Municipal Hospital, he had been promoted to full professor, and he was hiring his own research faculty. One of the scientists whom he brought into his laboratory was Julius S. Youngner (AAI '50) from the University of Michigan, who, as a senior assistant research scientist at the National Cancer Institute, had specialized in cell culture techniques. Youngner would remain an active member of the Pitt faculty for the next 50 years.
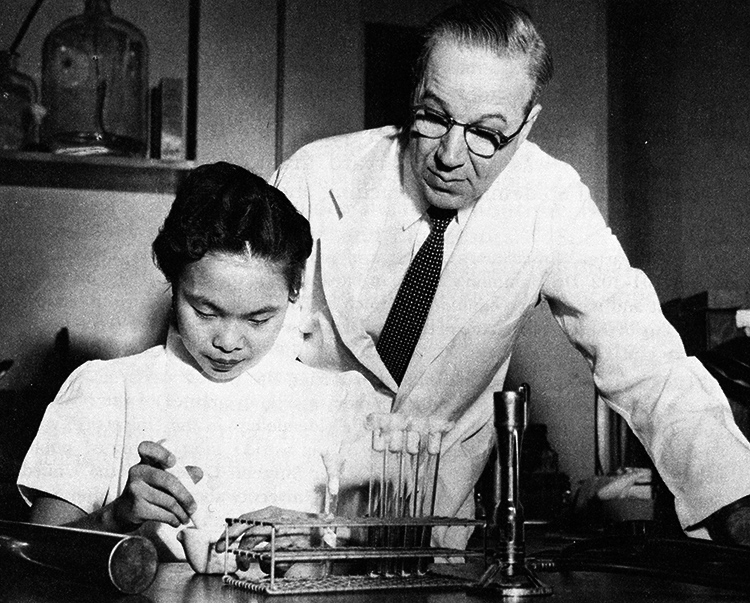 William McDowall Hammon
William McDowall Hammon
© University of PittsburghBy 1951, Salk’s laboratory had completed its typing project, concluding that there were three distinct types of poliovirus. The lab shifted its efforts to producing a vaccine. Based on the success that his mentor Francis had had with a killed-virus flu vaccine, Salk chose to pursue a killed-poliovirus vaccine over the attenuated-virus vaccine that the majority of other scientists, including his rivals Albert B. Sabin (AAI '46) and Hilary Koprowski (AAI '46), preferred.
Even within the small community of researchers at Pitt, Salk had competition. In 1950, Parran recruited William McDowall Hammon (AAI '46) to chair the Department of Epidemiology and Microbiology at the Graduate School of Public Health. Unlike Salk, who had no experience with polio research when he was hired to head the Virus Research Laboratory, Hammon had already established himself in the field when Parran convinced him to leave his position as dean of the School of Public Health at the University of California, Berkeley, for Pittsburgh. Wary of both killed-virus and attenuated-virus vaccines, Hammon preferred passive immunization through gamma-globulin injections containing polio-resistant antibodies. He conceded that passive immunization would not prevent infection, but he argued that it could prevent the worst symptom of infection—paralysis. NFIP-funded, double-blind trials involving more than 50,000 children in 1951 and 1952 yielded compelling evidence that passive immunization was a major step in the war against polio. Unfortunately, as Hammon himself pointed out, the immunity produced was only temporary, and the gamma- globulin was in short supply.
 Jonas Salk inoculating a young girl
Jonas Salk inoculating a young girl
National Library of MedicineMeanwhile, Hammon’s passive immunization approach was eclipsed by Salk’s March 1953 announcement of the successful completion of the first human trials of his group’s killed-virus vaccine. The national field trial, which involved more than 1.8 million children and was overseen by Thomas Francis, commenced in June 1954, and, on April 12, 1955, Francis pronounced the vaccine safe and effective. Salk instantly became a celebrity scientist, receiving a Presidential Citation and the Congressional Gold Medal in 1955 and the Albert Lasker Clinical Medical Research Award the following year. Although Salk left Pitt to head the Salk Institute in 1963, his accomplishments of the 1950s cemented Pitt’s reputation as a major research center for medical sciences.
Frank Dixon and the “Pittsburgh Five”
In addition to attracting national attention through his own laboratory studies, Salk’s administrative work helped contribute to the effort to transform Pitt into a major research institution. As the head of the search committee for a chair of the Department of Pathology in the medical school in 1951, Salk selected a scientist who shared several key characteristics with him: Frank J. Dixon was young, ambitious, and not yet well-known.
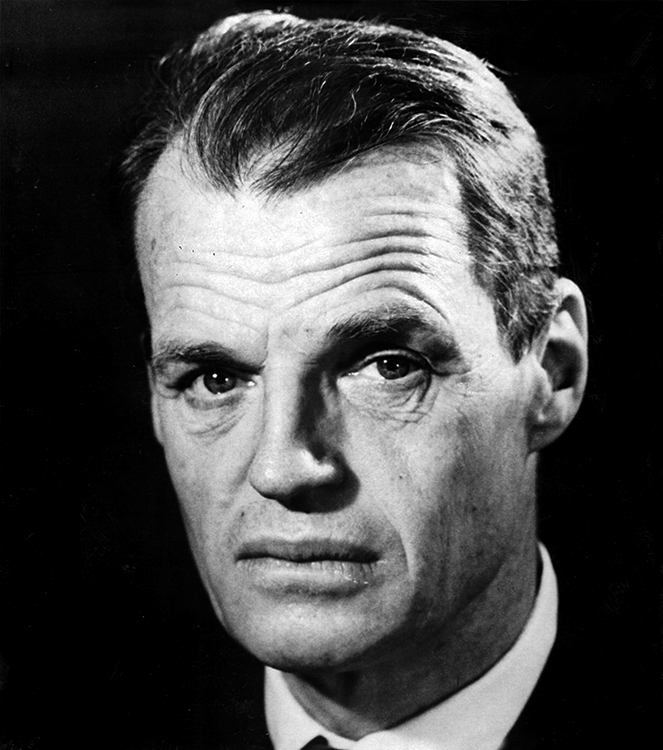
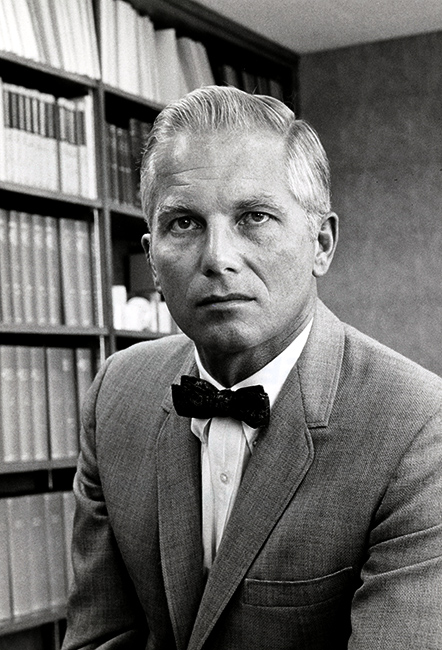 Frank J. Dixon
Frank J. Dixon
AAI Collection, UMBCDixon had grown up in St. Paul, Minnesota, and had attended the University of Minnesota, where he earned his M.D. in 1942 before entering the medical corps of the U.S. Marine Corps and serving in the Pacific Theater. Upon his return to the United States in 1946, Dixon became a research assistant in the Department of Pathology at Harvard. He moved to St. Louis, Missouri, in 1948, where he was an instructor in the Department of Pathology at Washington University for two years before being promoted to assistant professor in 1950. The following year, Salk and his search committee offered a full professorship and the chair of the Department of Pathology to Dixon, who, at age 31, became the youngest department head at Pitt.
As a research assistant at Harvard in 1946, Dixon had developed a new technique for labeling and tracking the location of proteins in the body using radioactive iodine. At Pitt, he used this procedure to study serum sickness and soon discovered that the host’s antibody immune response to foreign proteins in the injected serum caused deposition of immune complexes in tissues that led to tissue destruction. From these results, Dixon made a novel and important conclusion—the body’s immune response could have deleterious effects on the health of the host. Dixon’s careful methodology in the study of serum sickness and kidney disease served as a paradigm for immune complex- mediated disease pathogenesis and established the field of immunopathology, a discipline critical to the understanding of autoimmune diseases, such as lupus erythematosus and rheumatoid arthritis.
 The “Pittsburgh Five,” (L to R) Cochrane, Feldman, Dixon, Vazquez, and Weigle
The “Pittsburgh Five,” (L to R) Cochrane, Feldman, Dixon, Vazquez, and Weigle
The Scripps Research InstituteIn his second year at Pitt, Dixon received the Theobald Smith Award of the American Association for the Advancement of Science, an honor bestowed upon the most outstanding medical researcher under the age of 35. As chair of the pathology department, he sought to change the culture of the department so that it reflected both his youth and his interest in research. He brought in young scientists as fellows and assistant professors and allowed them to devote themselves to laboratory research by hiring part-time faculty to take care of many of the teaching and clinical responsibilities. Dixon believed that enthusiasm for research was contagious, explaining, "Nothing is more valuable than for a student to sit down and talk to a young researcher, six or seven years his senior, and feel the excitement that comes from scientific inquiry." One instance in which Dixon's teaching philosophy bore fruit was in the case of William O. Weigle (AAI '57), a laboratory technician from a working-class family, whom Dixon encouraged to pursue a Ph.D. at Pitt.
In 1960, Dixon received an offer from Edmund Keeney, director of the then relatively unknown Scripps Clinic in La Jolla, California, to establish a Division of Experimental Pathology. As long as Dixon could secure outside funding, he and his researchers would be free of administrative and teaching responsibilities and devote themselves to full-time research. Dixon, Weigle, Charles G. Cochrane (AAI '61), Joseph D. Feldman (AAI '63), and Jacinto "Joe" Vazquez (AAI '59)- known as the "Pittsburgh Five"-left Pitt for the Scripps Clinic in 1961, taking with them six post-docs and several members of the support staff. Together, they laid the foundation for the world-renowned Scripps Research Institute. Dixon's pioneering achievements in immunopathology were formally recognized when he was awarded the Gairdner Foundation International Award in 1969 and the Albert Lasker Basic Medical Research Award in 1975.
F. Sargent Cheever
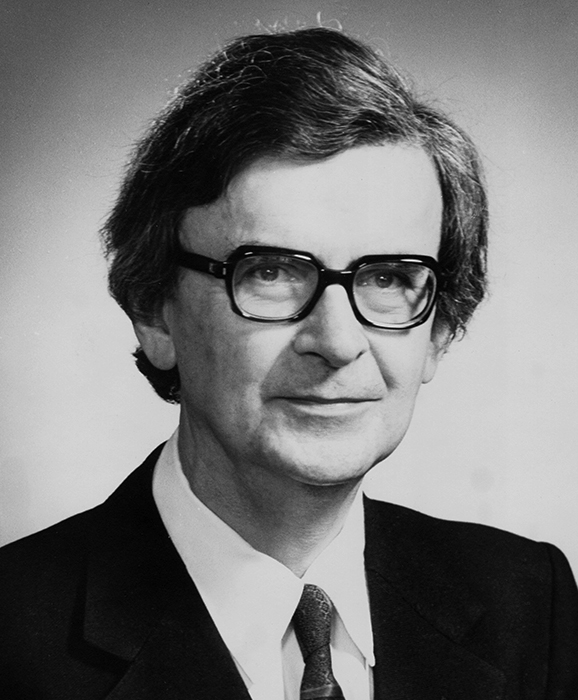
 Francis Sargent Cheever, c. 1962
Francis Sargent Cheever, c. 1962
AAI Collection, UMBCWhen William McEllroy retired in 1958, he was succeeded as dean of the School of Medicine by Francis Sargent Cheever. A fourth-generation Boston physician, Cheever attended the prestigious Groton School and received both his B.A. and M.D. from Harvard University. Following a two-year medical internship at Presbyterian Hospital in New York, he returned to Harvard in 1939 as a research fellow in bacteriology, rising to the rank of assistant professor by 1946. In 1950, acceding to an invitation from his Harvard classmate William Hammon to join him at Pitt, Cheever became a professor of epidemiology and microbiology in the Graduate School of Public Health.
Shortly after arriving at Pitt, Cheever sought a second appointment in the Department of Bacteriology in the School of Medicine. Eager to add another first-rate researcher to the medical school faculty and to further the relationship between the medical and public health schools, McEllroy made Cheever a lecturer in the Department of Bacteriology in 1951. Cheever was well-liked by his colleagues in both schools, and his patrician background allowed him to run in the same social circles as wealthy Pittsburgh donors who soon looked to Cheever as a spokesman for the university. These qualities led Parran to encourage Cheever to prepare for a role in administration, so when McEllroy announced in January 1958 that he would retire at the end of the term, Cheever was a natural choice as his successor.
Cheever excelled in the position and oversaw the expansion of the medical school during his 11-year tenure. The highlight of these years was the formal integration of the medical and public health schools with several Pittsburgh hospitals into the University Health Center [now the University of Pittsburgh Medical Center (UPMC)]. From 1970 to 1974, Cheever served as president of the new medical center.
Niels Jerne
 Niels K. Jerne
Niels K. Jerne
FASEB ArchiveAs dean of the School of Medicine, Cheever succeeded in attracting stellar faculty to Pitt, including Niels K. Jerne, who became chair of the Department of Microbiology in the School of Medicine in 1962. Jerne had already established himself as a preeminent immunologist at the time of his arrival. He had been a researcher at the State Serum Institute in Copenhagen for 10 years before joining Max Delbriick's laboratory at the California Institute of Technology in 1954, where he published the landmark paper, “The Natural-Selection Theory of Antibody Formation” in 1955. Jerne next headed the Biological Standards and Immunology sections of the World Health Organization in Geneva from 1956 to 1962, but, wishing to return to academic life and his immunological research, he seized the opportunity to chair the Department of Microbiology at Pitt when it arose in 1962.
The change of venues paid immediate dividends. Jerne, regarded as one of immunology’s greatest theorists, returned to the laboratory and made an important technical innovation. With Albert A. Nordin (AAI '72), a post-doc at Pitt, he developed the plaque-forming cell assay—often called the Jerne plaque assay— which advanced the study of immunology at the cellular level by allowing researchers to see and enumerate antibody-producing cells in an agar plate.
Jerne left Pittsburgh in 1966, succeeded at Pitt by Julius Youngner, who chaired the Department of Microbiology from 1966 to 1989. Jerne returned to Europe and directed the Paul Ehrlich Institute before becoming the founding director of the Basel Institute for Immunology in 1969. In recognition of his major contributions to the field of immunology, he was awarded the 1984 Nobel Prize in Physiology or Medicine.
New Directions: 1980s–Present
Neither the growth of the medical sciences at Pitt nor the role of AAI members in advancing it ended in the 1960s. Donald N. Medearis (AAI '65) succeeded Cheever as dean of the medical school, serving from 1969 to 1974. One of his most significant acts as dean was recruiting Thomas Detre to head the Department of Psychiatry in 1974.
As senior vice chancellor of the health sciences from 1984 to 1998, Detre left a lasting legacy on UPMC. He oversaw the transformation of UPMC into a research hub of international renown by establishing several research institutes, including the Pittsburgh Transplantation Institute (renamed the Thomas E. Starzl Transplantation Institute in 1996) and the University of Pittsburgh Cancer Institute (UPCI) in 1985.
 Olivera Finn, 2009
Olivera Finn, 2009
AAI ArchiveUnder the direction of Ronald B. Herberman (AAI '69), UPCI was designated a Comprehensive Cancer Center by the National Cancer Institute, five years after its establishment, making it the youngest center to receive such a distinction. Moreover, it was at UPCI that immunology began to emerge as one of the more significant areas of basic research at Pitt in the late 1980s. By 1997, the interdepartmental Graduate Program in Immunology had received accreditation and was authorized to award Ph.D. degrees. In January 2002, the School of Medicine established the Department of Immunology and appointed Olivera J. Finn (AAI '83, president 2007– 2008) its founding chair.
Although there is now a permanent home for the study of immunology at Pitt, studies in the field and AAI members remain ensconced in several departments and institutes across the university. Since 1997, Charles R. Rinaldo, Jr. (AAI '78), has served as chair of the Department of Infectious Diseases and Microbiology in the Graduate School of Public Health, the position once held by William Hammon. Recognizing parallels between the mid-century work on polio carried out by his predecessors at Pitt and his own research on HIV and AIDS, Rinaldo declared in a 2004 interview, “I look to history to help me look to the future.”
Salk, Dixon, Cheever, Jerne, and the many other AAI members who have called Pittsburgh home helped to establish the city as a major center for immunological research. In turn, Pittsburgh has contributed much to AAI. Five past presidents and one current councillor, Joanne L. Flynn (AAI '96, president 2018–2019), have spent at least some of their professional years in Pittsburgh. Beginning with Arthur Locke, who became an associate editor of The JI in 1936, Pittsburgh immunologists have worked to ensure that The JI remains the preeminent journal in the field, most notably Joseph Feldman, who served as editor-in-chief from 1971 to 1987. Together, these immunologists have left behind an enduring legacy that continues to inform the work of immunologists the world over.
References
- Askonas, Brigitte A., and James G. Howard. “Niels Kaj Jerne, 23 December 1911–7 October 1994.” Biographical Memoirs of Fellows of the Royal Society 43 (1997): 242–243.
- Brignano, Mary. Beyond the Bounds: A History of UPMC. Pittsburgh: UPMC, 2009.
- “Cheever, Francis Sargent.” American Men and Women of Science, 14th ed. (1979), 2:801.
- Dixon, Frank J., Jacinto J. Vazquez, William O. Weigle, and Charles G. Cochrane. “Pathogenesis of Serum Sickness.” A.M.A. Archives of Pathology 65, no. 1 (1958): 18–28.
- Finn, Olivera J., and Russell D. Salter. “Immunology in Pittsburgh.” Immunologic Research 36, nos. 1–3 (2006): 1–2.
- Greenberg, Daniel S. “The Vanishing Heroes of Science.” New York Times, July 4, 1995.
- Hart, Peter. “Obituary: Thomas P. Detre.” University Times [University of Pittsburgh]. October 14, 2010.
- Jerne, Niels K. “The Natural-Selection Theory of Antibody Formation.” Proceedings of the National Academy of Sciences of the United States of America 41, no. 11 (1955): 849–857.
- Jerne, Niels K., and Albert A. Nordin. “Plaque Formation in Agar by Single Antibody-Producing Cells.” Science 140, no. 3565 (1963): 405.
- Kauffman, Leah. “California Dreaming: Frank Dixon Dreams Immunopathology and White Sand Beaches.” Pitt Med. January 2002.
- Lacy, G. R., and C. C. Hartman. “Specific Reactions of the Body Fluids in Pneumococcic Infections.” The Journal of Immunology 3, no. 1 (1918): 43–49.
- Lloyd, Erica. “Challenging Cowboys: An Immunologist Rides into the Sunset.” Pitt Med. October 2001.
- Oldstone, Michael B. A. “Frank James Dixon, 1920–2008.” Biographical Memoirs Washington, DC: National Academy of Sciences, 2009.
- Oshinsky, David M. Polio: An American Story. New York: Oxford University Press, 2005.
- Paull, Barbara I. A Century of Medical Excellence. Pittsburgh: University of Pittsburgh Medical Alumni Association, 1986.
- Pifer, Jenelle. “We Knew You When: Charles Cochrane and the Pittsburgh Five.” Pitt Med, Fall 2012, 39.
- Rinaldo, Charles R., Jr. “Passive Immunization against Poliomyelitis: The Hammon Gamma Globulin Field Trials, 1951–1953.” American Journal of Public Health 95, no. 5 (2005): 790–799.
- Salk, Jonas E. “Studies in Human Subjects on Active Immunization against Poliomyelitis. 1. A Preliminary Report of Experiments in Progress.” Journal of the American Medical Association 151, no. 13 (1953): 1081–1098.
- Warren, Shields, and Frank J. Dixon. “Antigen Tracer Studies and Histologic Observations in Anaphylactic Shock in the Guinea Pig.” American Journal of the Medical Sciences 216, no. 2 (1948): 136–45.
- Weigle, William O., and Frank J. Dixon. “Relationship of Circulating Antigen-Antibody Complexes, Antigen Elimination, and Complement Fixation in Serum Sickness.” Experimental Biology and Medicine 99, no. 1 (1958): 226–231.
- “About.” Graduate School of Public Health, University of Pittsburgh. http://www.publichealth.pitt.edu/home/about (accessed August 6, 2018).
- “Oscar Teague.” The Journal of Immunology 9, no. 1 (1924): 1–5.
- “Pitt Names New Dean of Medicine.” Press Release. January 30, 1958. Documenting Pitt, University of Pittsburgh.
- “Text of the Statements on Dr. Salk’s Vaccine Evaluation.” New York Times. April 13, 1955.
- “Unsung Hero of the War on Polio.” Public Health [University of Pittsburgh Graduate School of Public Health]. Spring 2004.